Menstrual Cycle Tracking Benefits
Women have been experiencing the ebbs and flows of their menstrual cycles for centuries. However, we have only recently begun to truly understand and appreciate the importance of tracking these
Women have been experiencing the ebbs and flows of their menstrual cycles for centuries. However, we have only recently begun to truly understand and appreciate the importance of tracking these

Are you considering starting a family? Whether you’ve been contemplating pregnancy for a while or have just made the decision, it’s likely an exciting moment in your life! Getting pregnant

What is Cervical Mucus? Cervical Mucus is fluid produced and released from the cervix. The consistency of cervical mucus can vary based on the day of your menstrual cycle (based

There is no such thing as a perfect birth control solution. There are other factors to consider, such as convenience, efficacy, and cost. Find out how to choose the best

What happens now that you’ve decided to build a family? There are easy things you can do right now to get a jump start on family planning. It’s not always

It’s that time of the month again. You’ve probably proclaimed that your period is the absolute worst at one point in your life. What your period says about your health

Q. What is a Holistic Approach? A holistic approach to modern medicine is characterized by treating the person as a whole, rather than treating specific diseases or symptoms. This approach
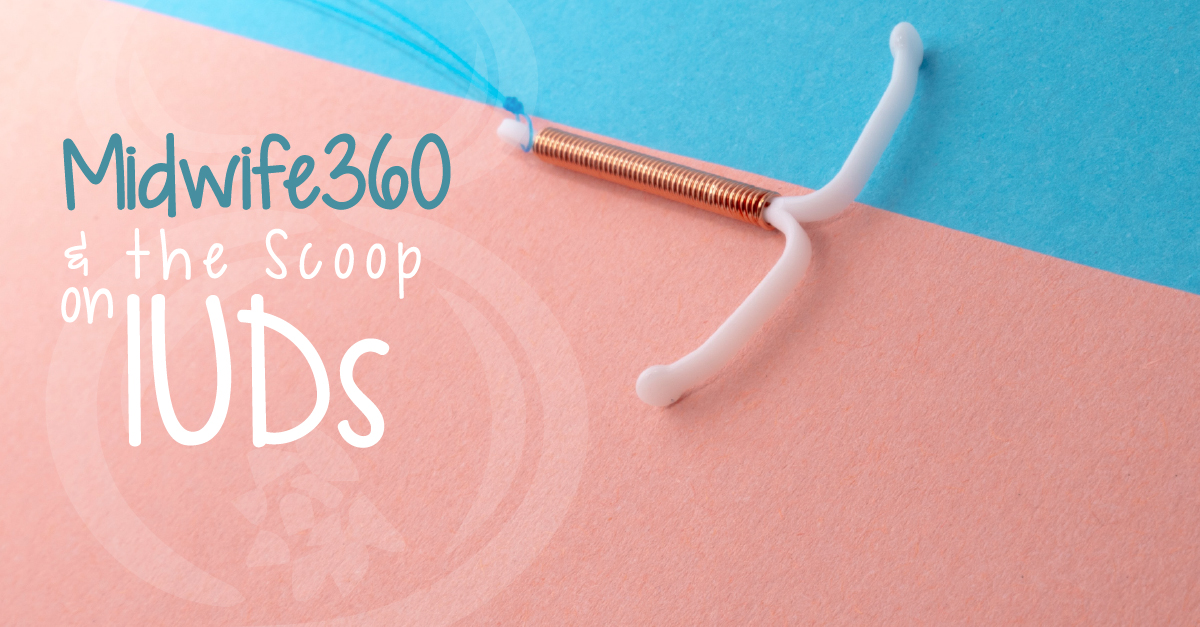
Many of my clients ask about birth control options that do not have hormones. There are a few, mostly they are the barrier methods like condoms (male and female), diaphragms, and cervical caps, or surgery. But the copper IUD is the only one that is long term and reversible and does not have any hormones. Since the copper IUD is not the only long term, reversible contraceptive, I wanted to break it down here for you.

It is well known that the American childbirth culture is very expensive with very poor performance AND little of what happens to birthing people in hospitals is evidence-based.

Health Insurance A Lose:Lose Situation for Consumers and Providers

When it comes to childbirth, high tech is not better than low tech. I have been privileged to attend many out of hospital births and many more in hospital births. Even a ‘normal’ birth in the hospital typically comes with continuous fetal monitoring and epidural.

My name is Fadwah Halaby and I am a certified nurse midwife serving families in
Can I have a vaginal birth if I already had a c section? The short answer is, “YES! YOU CAN!” While the long answer requires a conversation about various risks – risks of a VBAC, or vaginal birth after cesarean, AND risks of repeat surgery.

Let me tell you a story… Let’s talk about what’s wrong with the current Medical
